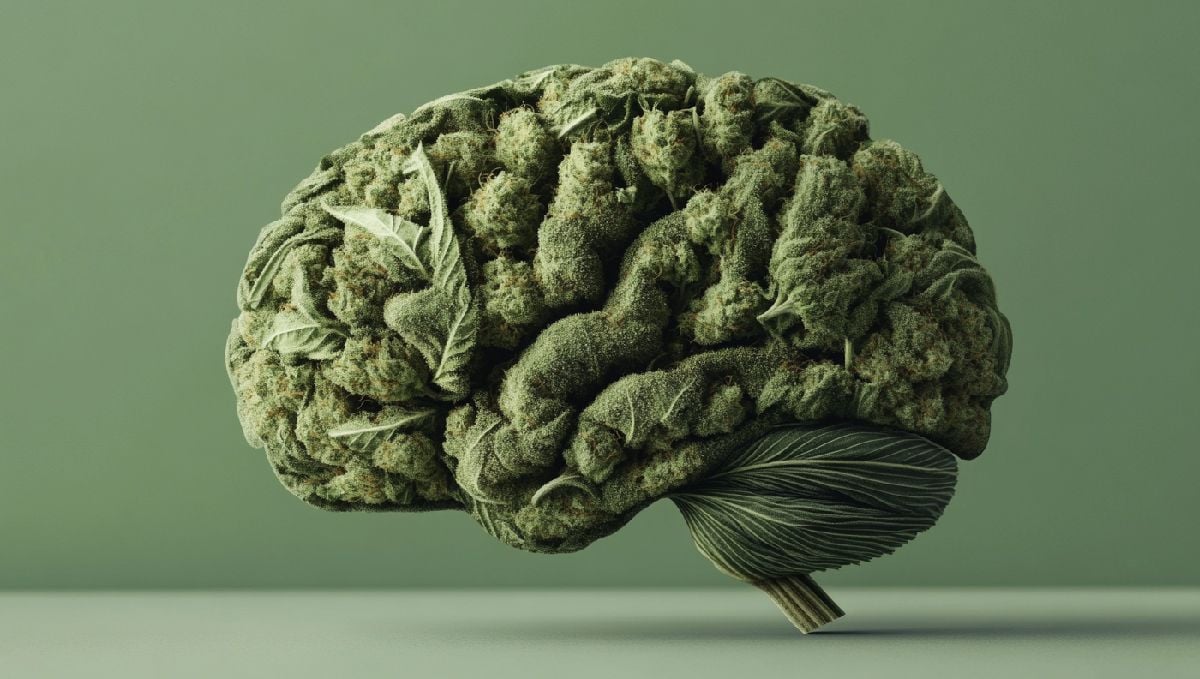
Is Cannabis Addictive? Here’s What The Research Tells Us

- 1. Is marijuana addictive?
- 2. Cannabis addiction risk
Separating truth from fiction, our readers want to know– is cannabis addicitve?
The messaging that cannabis is a “gateway drug” or addictive are myths that have followed the plant for a century due to its prohibition. There is no data that backs up cannabis being a gateway to worse drugs. Beginning in the early 1900s in most countries around the world, a push for weed prohibition created fear mongering around the plant that wasn’t based on science. These sentiments were based on control and fear, often policing classes as well as the consciousness of the population.
Today, as the research of cannabis becomes legalized in many countries across the world, we are seeing emerging data that suggests cannabis is not addictive. Further, it also shows that consumers can even use weed as a recovery tool from addiction to more dangerous substances like alcohol and pharmaceuticals. Cannabis is actually a way to recover from more harmful and physically addictive substances and shows a beacon of light to help people out of the opioid crisis.
Here’s what the current data says on cannabis addiction risk.
Is Marijuana Addictive?
There is not enough peer-reviewed, controlled studies to say whether cannabis is addictive or not. What we do know is that it is impossible to overdose on cannabis.

There are genetic studies that suggest developing cannabis addiction is hereditary, doctors at Yale Medicine write. These authors also claim that more research is needed to determine reliability. One Harvard doctor who has dedicated his career to debunking myths on cannabis, Dr. Peter Grinspoon, writes about several studies that show evidence of CBD as helpful for people suffering from addiction to opioids, mostly by reducing anxiety. “We need better data, but I believe that CBD (and I believe full cannabis as well) will have a growing role as an adjunct treatment for people suffering from opioid addiction,” writes Dr. Grinspoon.
Cannabis Addiction Risk
One 2018 review that’s often cited found: “Although further research is necessary, the findings summarized here indicate that neurobiological changes in CUD seem to parallel those in other addictions, albeit to a lesser extent in some brain systems.”
The review does admit that the existing research on cannabis and addiction has holes in it. This review listed the questions we need to ask and gain more data on in order to know if cannabis is addictive. Questions for future research include:
- Do changes in CBIR density after abstinence from cannabis parallel changes in target receptors of other drugs of abuse?
- Are behavioral and mood variations associated with cannabis use a risk factor or consequence of cannabis addiction?
- Are long-term behavioral and neurophysiological changes related to the THC content in cannabis?
- Is cannabis use associated with long-term changes in glutamate signaling as seen in other drugs of abuse?
- Is cannabis use associated with disruptions in the amygdala and habenula as seen with other drugs of abuse?
According to the American Center for Disease Control, 9% of adults who use cannabis for a long period will develop “cannabis use disorder.” The definitions of CUD are widely ranging and not agreed upon by physicians. It’s important to keep in mind that cannabis doesn’t come with the same physical withdrawal symptoms as other substances, including alcohol. The withdrawls of cannabis are mild discomfort. For this reason, it doesn’t have the same harmful characteristics of other substances.
One 2020 study looking at 23,000 participants found the prevalence of cannabis withdrawal syndrome at 47%. The study reads: “Factors that were associated with higher cannabis withdrawal syndrome were clinical settings (particularly inpatient and outpatient vs population settings), concurrent tobacco or other substance use, and daily cannabis use.”
The definition of cannabis withdrawal symptoms is very widely ranging and often contested by doctors today. It includes any of these symptoms: irritability, anger, or aggression; nervousness or anxiety; sleep disturbance; appetite or weight disturbance; restlessness; depressed mood; and somatic symptoms, such as headaches, sweating, nausea, vomiting, or abdominal pain. These symptoms are mild. I believe they reflect the benefit of cannabis on our nausea, sleep, and mood, as opposed to the harm of cannabis withdrawal. More studies need to look at a larger demographic of people and in controlled environments to determine if cannabis withdrawal syndrome is this prevalent.
The War on Drugs has had its effect on the existing cannabis research on this topic. Cannabis has simply never been studied, so much of the research we have shows its harm as opposed to its benefits. In the future, more peer-reviewed studies are needed to show if this is reliable data.












Comments